
Validation of the Spanish Version of the Parent Diabetes Distress Scale
[Validación de la versión española de la escala Parent Diabetes Distress]
Marina Beléndez1 and Lawrence Fisher2
1University of Alicante, Alicante, Spain; 2University of California, San Francisco, United States of America
https://doi.org/10.5093/clh2025a3
Received 13 June 2024, Accepted 22 October 2024
Abstract
Background: Type 1 diabetes is a chronic condition that presents significant challenges not only for affected children and adolescents but also for their parents. The study examined the psychometric properties of the Spanish version of the Parent Diabetes Distress Scale (PDDS-SP) for parents of children and adolescents with type 1 diabetes. Method: Data were collected on 314 parents recruited through diabetes associations and Facebook groups. Participants completed the PDDS-SP, a well-being measure, and provided information about their child’s diabetes and treatment. Results: Exploratory factor analyses identified a 16-item, four-factor structure: parent-child relationship concerns, personal distress, distress about the child’s diabetes self-management, and health care team concerns. Cronbach’s alpha indicated adequate reliability. Higher PDDS-SP scores were associated with lower well-being and more frequent hypoglycemic episodes. Mothers reported higher distress than fathers. Conclusions: The PDDS-SP was found to be a reliable and valid measure for assessing diabetes-related distress among Spanish-speaking parents.
Resumen
Antecedentes: La diabetes tipo 1 es una enfermedad crónica que presenta retos no sólo para los niños afectados, sino también para sus padres. El estudio examinó las propiedades psicométricas de la versión española de la Escala de Distrés en la diabetes para padres (PDDS-SP) de niños y adolescentes con diabetes tipo 1. Método: Se recogieron datos de 314 padres reclutados a través de asociaciones de diabetes y grupos de Facebook. Los participantes completaron el PDDS-SP, una medida de bienestar, y proporcionaron información sobre la diabetes y el tratamiento de sus hijos. Resultados: El análisis factorial exploratorio obtuvo 16 ítems y cuatro factores: preocupación por la relación progenitor-hijo, distrés personal, distrés por el manejo de la diabetes y preocupación por el equipo sanitario. El alfa de Cronbach indicó una fiabilidad adecuada. Puntuaciones más altas del PDDS-SP se asociaron a menor bienestar y a episodios hipoglucémicos más frecuentes. Las madres manifestaron mayor distrés que los padres. Conclusiones: El PDDS-SP es una medida fiable y válida para evaluar el distrés relacionado con la diabetes en progenitores españoles.
Palabras clave
Padres, Niños, Adolescentes, Distrés por la diabetes, Diabetes tipo 1, Análisis factorialKeywords
Parents, Children, Adolescents, Diabetes distress, Type 1 diabetes, Factor analysisCite this article as: Beléndez, M. & Fisher, L. (2025). Validation of the Spanish Version of the Parent Diabetes Distress Scale. Clinical and Health, 36(1), 19 - 24. https://doi.org/10.5093/clh2025a3
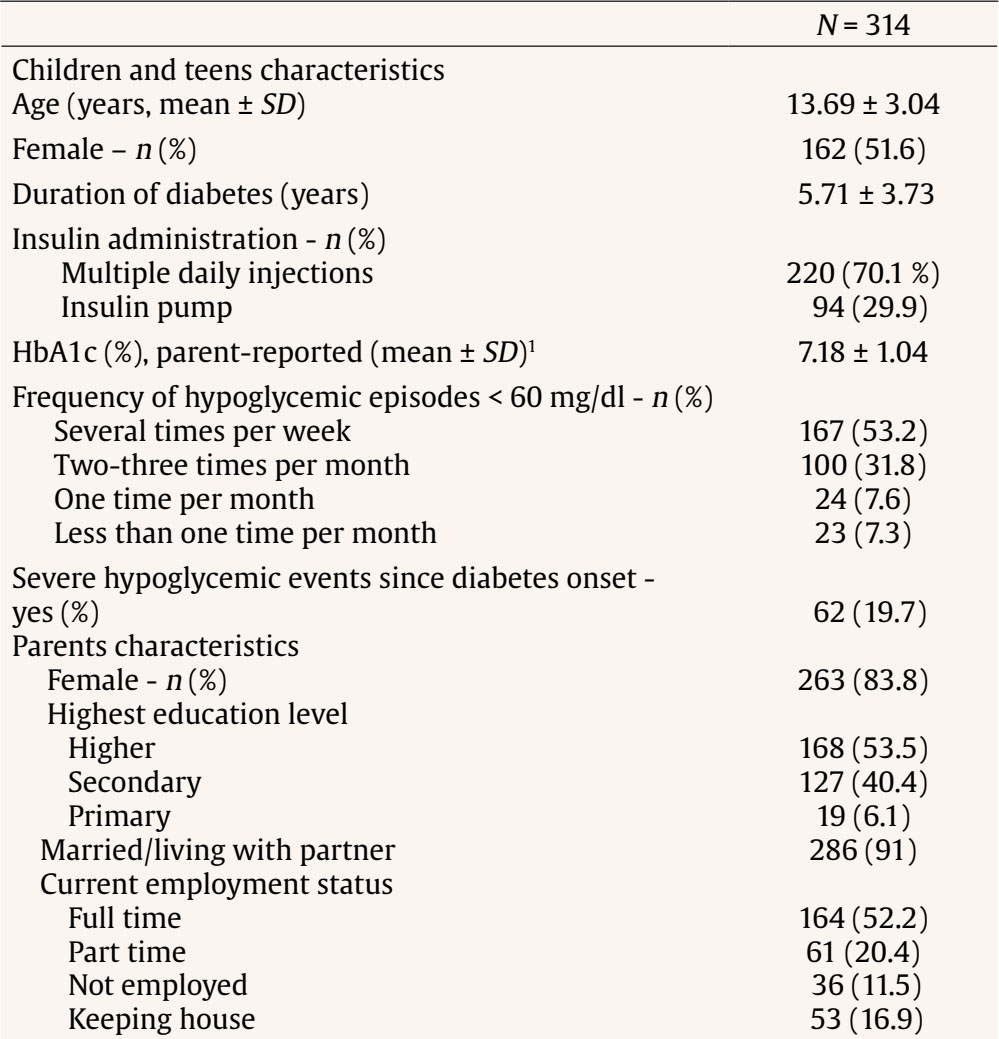
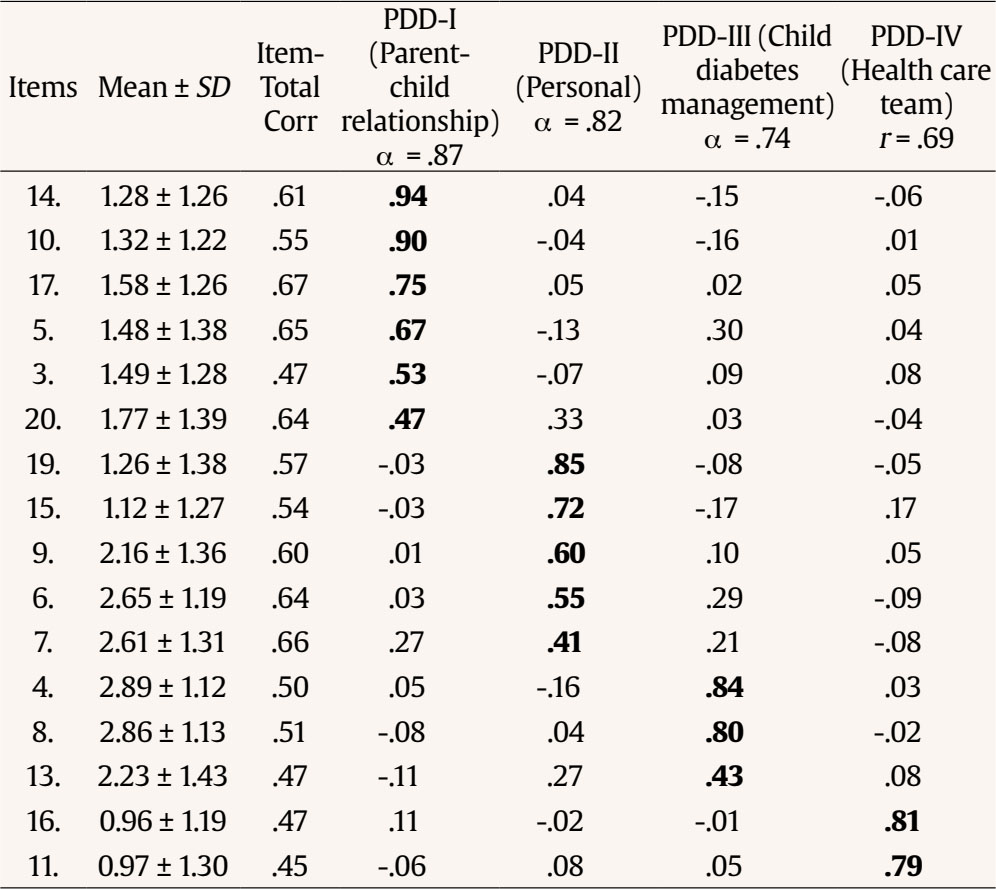
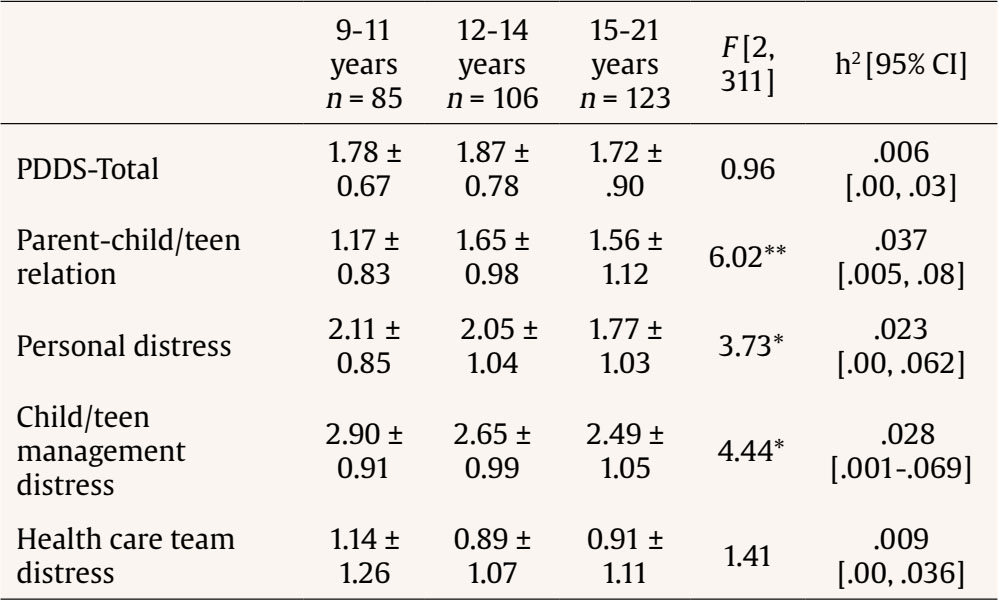
Correspondence: marina.belendez@ua.es (M. Beléndez).Type 1 diabetes is a condition in which the body stops producing insulin. One of the goals of diabetes care is to maintain glucose levels within the target range to prevent hypoglycemia and long term complications. Managing the disease involves daily tasks such as administering insulin (multiple daily injections or insulin pump), monitoring blood glucose levels, following a meal plan and exercising regularly (March et al., 2023). Diabetes distress is an emotional response to living with diabetes and the daily burden of managing the disease (Skinner et al., 2020). Managing blood sugar levels and concerns about hypoglycemia are common sources of distress for parents of children with type 1 diabetes (Lindström et al., 2017; Markowitz et al., 2012; Whittemore et al., 2012). As children reach school age, parents often face new worries regarding their child’s diabetes care while away from home. Diabetes care becomes a shared responsibility between adolescents and their parents during this stage, which can lead to disagreements and conflicts (Law et al., 2013; Streisand et al., 2005). Regardless of their children’s age, parents may feel frustrated and isolated in caring for their children’s diabetes (Kimbell et al., 2021). Research has shown that diabetes distress may have negative consequences for parents’ psychological well-being, as it has been linked to the development of depressive symptoms (Noser et al., 2019). Diabetes distress can not only affect parents but also impact the disease management and glycemic control of their children. Worried parents may exhibit controlling behavior, hindering their children’s involvement in diabetes care (Jaser, 2011). Conversely, overwhelmed parents may transfer responsibility to their children prematurely, which could have adverse effects on disease management (Palmer et al., 2004). Also, several studies have found that high levels of parental distress are associated with poorer glycemic control in their children (Beléndez, 2018; Hessler et al., 2016). Therefore, it is crucial to assess parent diabetes distress to better understand how parents cope with the challenges of diabetes management and its impact on the child’s diabetes care. The pioneer instrument in the assessment of parent diabetes distress is the PAID-PR (Problem Areas in Diabetes - Parent Revised) scale (Markowitz et al., 2012), adapted from the PAID scale for adults (Polonsky et al., 1995). The PAID-PR scale includes items related to emotional reactions and concerns about the care and adaptation of their children to diabetes, caregiver burden or exhaustion, and the perception of a lack of support to cope with that excessive demand. In the validation study of the Spanish version of the PAID-PR mothers reported higher levels of distress than fathers (Beléndez, 2018). Recently, separate versions of the PAID have been validated for use with parents of children (P-PAID-C; Evans et al., 2019) and parents of adolescents (P-PAID-T; Shapiro et al., 2018). Although these scales assess various facets of parent diabetes distress, they do not thoroughly evaluate parents’ concerns about their relationship with their child or adolescent, including diabetes-related disagreements, which become a relevant aspect during late childhood (9-11 years) when children have already acquired autonomy in most illness management tasks (Schilling et al., 2006). To overcome this limitation, the Parent Diabetes Distress Scale (PDDS) was developed in the United States to comprehensively assess four domains of diabetes distress in parents of adolescents (Hessler et al., 2016). These areas include Parent-Child Relationship Distress, reflecting concerns about conflicts and disagreements with their teen related to diabetes, Personal Distress, covering frustration and emotional strain parents feel due to their child’s diabetes, including a lack of support or feeling overwhelmed, Child Management Distress, addressing worries about their teen’s diabetes, such as hypoglycemia, and Health Care Team Distress, relating to concerns about whether their child was receiving the medical attention needed. The PDDS was specifically designed for use with American parents of teenagers aged 11-21 years and its validity has not been evaluated in samples of parents with younger children or in other cultural contexts. However, upon reviewing the content of the scale, it appears that the PDDS could also be suitable for parents of children in the late childhood or pre-adolescence stage (9-11 years). Thus, the aim of this study was to assess the psychometric properties of a Spanish version of the PDDS (PDDS-SP) in a sample of parents with children diagnosed with type 1 diabetes ranging from late childhood to adolescence. In order to establish the validity of the PDDS-SP, and based on previous research (Beléndez, 2018; Hessler et al., 2016), we expected that higher PDDS-SP scores would be associated with lower parents’ well-being, more frequent hypoglycemic episodes and poorer blood glucose control. We also hypothesized that mothers would report higher PDDS scores than fathers (Beléndez, 2018; Haugstvedt et al., 2011). Moreover, we anticipated that parents of adolescents would express greater concern about conflicts or disagreements with their children regarding diabetes care compared to parents of younger children. Participants The inclusion criteria for this study were being a parent living in Spain with a child aged 9 to 21 years who had been diagnosed with type 1 diabetes for at least one year. Procedure To recruit parents, announcements containing a link to an online survey administered via Qualtrics were disseminated through several Spanish diabetes patients’ associations and Facebook groups for parents of children and adolescents with diabetes. Parents provided informed consent by checking a box before proceeding to answer the survey. Parents did not received any compensation for their participation. This study was approved by the Research Ethics Committee of the University of Alicante (Spain). Measures The survey included a number of measures. Parent Diabetes Distress Scale (PDDS-SP) Spanish Version The original PDDS (Hessler et al., 2016) version is consisted of 20 items (5-point scal, from 0 = not at all to 4 = a great deal) that refer to four areas of parent diabetes distress. Higher scores indicated higher levels of distress. The PDDS-SP was developed through a process of forward translation, synthesis, back translation, and review involving a pediatrician (bilingual), two professional translators (bilingual), two expert psychologists specializing in diabetes (fluent in Spanish), one researcher proficient in Spanish and English, and one of the original scale’s authors. In the review process, the item 18 was shortened by eliminating reference to health insurances concerns, because it was not considered applicable to the Spanish context. The original and Spanish versions of the PDDS are presented in Table 1. Table 1 English and Spanish Version of the Parent Diabetes Distress Scale  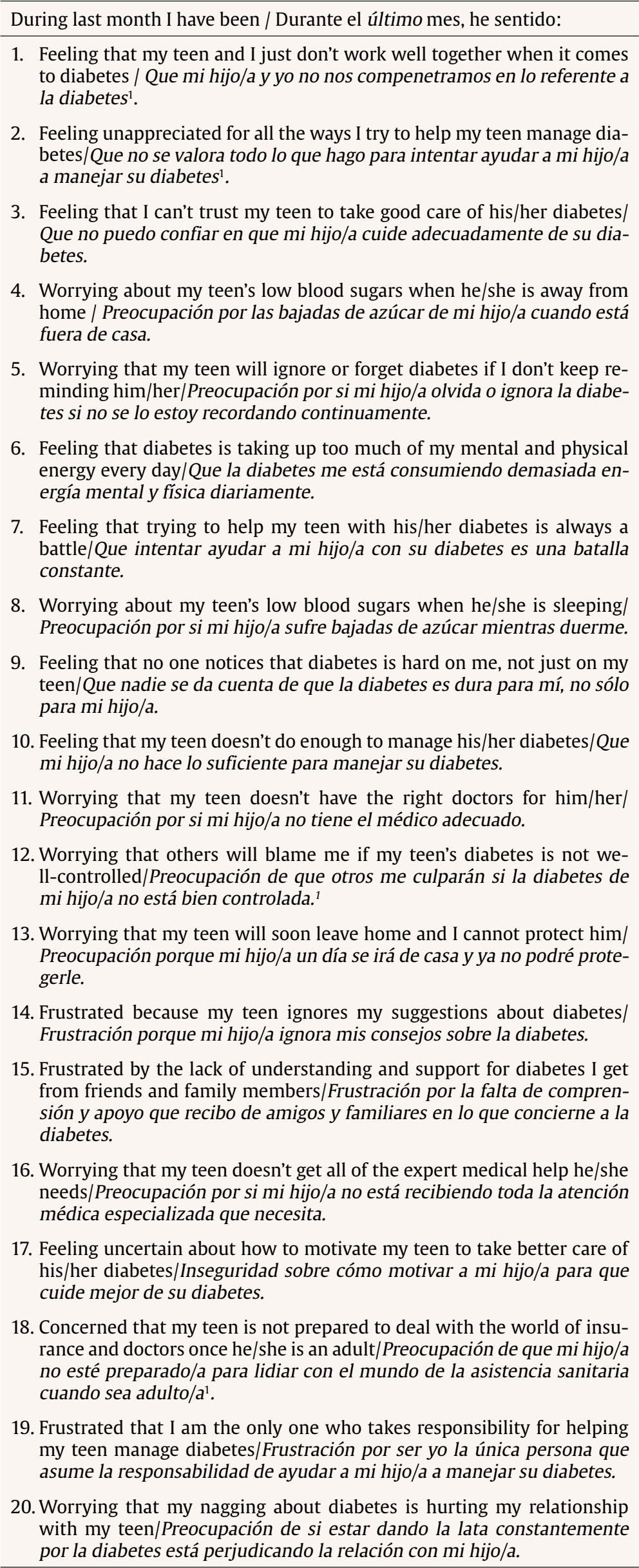 Note. 1Items deleted after factor analysis of the PDDS-SP. WHO Emotional Well-Being Index (WHO-5) Spanish Version This index (Sischka et al., 2020; Topp et al., 2015) was used to assess the emotional well-being of parents. The questionnaire is composed of 5 items (from 0 = never to 5 = all the time) which covered positive mood, vitality and general interests. The WHO-5 performs well in detecting mild to moderate levels of depression (Krieger et al., 2014). A high score indicates greater emotional well-being. The internal consistency of the scale in this sample was α = .88. Parent Demographic Characteristics Gender, partner status, education, and employment status were measured by several items. Questions about the child covered age, gender, and initials of first and last names. Parents also self-reported clinical data about the child, including the duration of diabetes, insulin administration method (multiple daily injections or pump), frequency of hypoglycemic episodes below 60 mg/dl (1 = never, 5 = several times per week), and the most recent HbA1c value (glycated hemoglobin, a measure of blood glucose control, reflecting average blood glucose levels over the past 2-3 months). Data Analysis When both parents of the same child completed the survey, only fathers’ responses were included for two reasons: to avoid correlated data in the analyses and because of the under-representation of fathers in the sample. To identify both parents of the same child, each participant was assigned a code based on the initials of their child’s first and last names, along with the child’s sex, age, and duration of diabetes. As one aim of the study was to examine the factor structure of the PDDS in a language in which it had not yet been used, an exploratory factor analysis (EFA) was performed. When a scale is translated into a different language, items may be grouped differently than in the original version or some items may not work well. Thus, EFA is generally considered more appropriate than confirmatory factor analysis (CFA) (Reichenheim & Moraes, 2007; Swami & Barron, 2019). To retain an item within a factor, a factor load ≥ .40 within a principal factor was required (Costello & Osborne, 2005). Cronbach’s alpha coefficient was determined to establish internal consistency. To examine validity, Pearson correlation coefficients were calculated between the PDDS-SP and the criterion measures: WHO-5 index, frequency of hypoglycemic episodes, and parent-reported most recent HbA1c value. To analyze differences in PDDS-SP scores according to parents’ gender t-tests were performed. One-way analysis of variance (ANOVA) with Tukey post-hoc analysis was performed to compare PDDS scores across three age groups based on their children’s age: late childhood (9-11 years), young adolescence (12-14 years) and older adolescence (15-21 years). The data analysis was carried out using IBM SPSS 26.0. A total of 324 parents of 314 children met the inclusion criteria. Thus, the final sample consisted of 314 participants (263 mothers and 51 fathers). Fifty-one percent of parents were recruited through Facebook parent groups, 40.4% through diabetes patients’ associations, and the remainder learned about the survey via Twitter or WhatsApp parent groups. Mean age of children was 13.7 years and mean duration of diabetes was 5.72 years. The demographic data of the parents and their children, as well as the data on their children’s diabetes and treatment, are shown in Table 2. As the forced response option was enabled in the online survey there were no missing data. In order to obtain evidence of construct validity, an EFA using principal axis factoring and Promax rotation was performed, Kaiser-Meyer-Olkin [KMO] index = .90; Bartlett’s sphericity test, χ2(190, N = 314) = 2999.78, p < .000. The initial five-factor solution suggested by eigenvalues ≥ 1 and inspection of scree plot was rejected because one factor was uninterpretable, so a four-factor solution was selected. After deleting four items (1, 2, 12, and 18) with loadings < .40 (see Table 1), a 16-items scale with four factors that accounted for 67.13% of the variance was obtained. All items except item 7 loaded on the same factors as in the original scale. Regarding the reliability of the PDDS-SP in the current sample, Cronbach’s alpha for the 16-item scale was .90. Intercorrelations among the subscales ranged from r = .34 to r = .58. Table 3 includes descriptive statistics for the items, item-total correlations, factor loadings after rotation, and reliability coefficients (Cronbach’s alpha) and correlation coefficient (for the two-item factor) for the extracted factors: parent-child relationship distress (PDD-I), personal distress (PDD-II), child management distress (PDD-III) and healthcare team distress (PDD-IV). The area that worried parents the most was related to their children’s diabetes management. Specifically, 71.4% of parents were very or extremely concerned about their children experiencing low blood sugar while away from home, 67.9% about low blood sugar while they were asleep, and 48% about their children leaving home for a day and being unable to protect themselves. Parents also scored high on items related to personal distress, with 58.6% of parents feeling (a lot/a great deal) that diabetes consumed too much of their daily mental and physical energy. Conversely, aspects related to the medical team were of least concern to parents. Concerning convergent validity, parents with higher PDDS-SP scores (both total and subscales) had lower well-being scores on the WHO-5. Regarding criterion-related validity, parents of children experiencing more frequent hypoglycemic episodes and poorer blood glucose control (higher HbA1c values) reported higher levels of diabetes distress (see Table 4). Table 4 Correlations between PDDS Total and Subscales with Other Measures  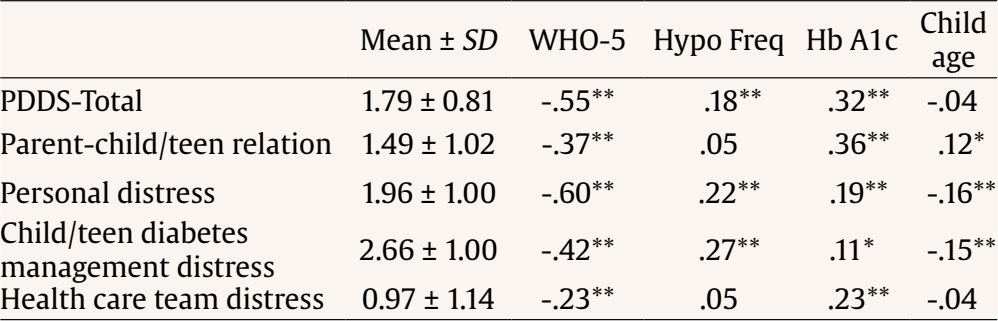 Note. SD = standard deviation; WHO-5 = WHO Well-being Index: M = 2.20 ± 1.07 Hypo Freq, frequency of hypoglycemic episodes < 60 mg/dl: M = 4.31 ± 0.91, HbA1c (n = 295): 7.18% (range 5.10-14). *p < .05, **p < .01. In addition, mothers reported higher levels of total DD (M = 1.85 ± 0.78) than fathers: M = 1.47 ± 0.88), t(312) = -3.07, p < .01. Specifically, gender differences were found in the subscales of personal distress, mothers: M = 2.05 ± 0.99; fathers: M = 1.48 ± 0.93; t(312) = -3.79, p < .000 and child diabetes management distress, mothers: M = 2.77 ± 0.97; fathers, M = 2.07 ± 0.96; t(312) = -4.70, p < .000. Finally, parents of adolescents had more concerns about their relationship with their children compared to parents of children in the late childhood stage, F(2, 311) = 6.02, p = .003, while parents of older adolescents perceived less diabetes management distress, F(2, 311) = 4.43, p = .013, and personal distress, F(2, 311) = 3.73, p = .025, than parents of younger children (see Table 5). This study aimed to assess the psychometric properties of the Spanish version of the PDDS among parents of children ranging from late childhood to adolescence. Except for one item, the factor structure of the PDDS-SP was similar to the original PDDS. The first factor, Parent-child Relationship Distress, represented parents’ concerns regarding disagreements and conflicts with their child. This subscale was originally composed of eight items, but for this study item 1 (“Feeling that my teen and I just don’t work well together when it comes to diabetes”) was removed due to low factor loading. Furthermore, item 7, which was part of this factor in the original version, loaded on a different factor in PDDS-SP. The second factor, Personal Distress, initially consisted of six items that measured parents’ concerns about their personal emotional well-being. However, in our study, two items (2 and 12) were removed and item 7, which was originally part of the first factor loaded onto the Personal Distress factor. This difference may be due to the broader interpretation of the word “battle”, which could refer to a constant personal struggle beyond conflicts with their children. The third factor of the original PDDS, Child Management Distress, included four items (4, 8, 13, and 18) that reflect parents’ worries about their child’s diabetes management. The original item 18 (“concerned that my teen is not prepared to deal with the world of insurance and doctors once he/she is an adult”), which had already been modified to make it more applicable to the context of Spanish healthcare was finally removed. The fourth factor, Healthcare Team Distress, consisted of the same two items as in the original PDDS. Thus, this shorter version of the PDDS (16 items) enhances its feasibility of application while retaining the original factorial structure. The Spanish version of the PDDS demonstrated adequate internal consistency, with both the total scale and its factors meeting the accepted threshold of .70 (Boateng et al., 2018). Our findings suggest that parental distress related to diabetes is a widespread issue, as most parents reported experiencing some level of diabetes distress. The average total PDDS-SP score almost reached 1.80 (2 = somewhat distress). As in the validation study of the original scale and in other previous studies on parental concerns of children with diabetes, the highest scored items were related to concerns about possible hypoglycemia (Child Diabetes Management Distress factor). The pattern of relationships between the PDDS-SP and demographic, diabetes and psychological variables, support the validity of the scale. As expected, mothers exhibited higher levels of distress than fathers. Today, women in families typically bear the burden of healthcare tasks, which means that mothers often assume greater responsibility for caring for their children’s diabetes. For example, mothers are more likely than fathers to reduce their working hours to take care of their young children with diabetes (Dehn-Hindenberg et al., 2021). This additional burden may partly account for their higher levels of diabetes distress, as reported in previous studies (Beléndez, 2018; Nieuwesteeg et al., 2017). Also, as expected, the level of concern about how diabetes could affect the relationship with their children was higher among parents of adolescent children than among parents of younger children. On the other hand, parents of children with a higher frequency of hypoglycemic episodes reported higher levels of diabetes distress, confirming our hypothesis. Our results also suggest positive correlations between PDDS-SP scores and HbA1c values. However, causality cannot be inferred from these results. The deterioration of glycemic control, which is often observed when children reach adolescence, may cause concern for parents. Additionally, parents’ diabetes distress may negatively impact the parent-child relationship, which could adversely affect diabetes management and lead to poorer glycemic control. Furthermore, parents with higher PDDS-SP scores (total and subscales) had lower scores in well-being (WHO-5), providing further evidence of the validity of the PDDS-SP. Our study has several limitations. First, half of the parents were recruited through Facebook groups for parents of children and adolescents with diabetes, which may affect the sample’s representativeness. However, we also recruited parents through diabetes patient associations, which typically attract a large number of parents, providing an effective way to reach our target population. This broader recruitment strategy may help reduce the potential biases associated with social media recruitment. Likewise, parents of children and adolescents with diabetes are increasingly joining or creating Facebook groups to connect with others in similar situations. These groups provide not only support for diabetes management but also a platform to discuss questions about new technological advances in diabetes care. In traditional recruitment methods, typically conducted through hospital consultations, recruitment often occurs at one or a few hospitals, resulting in a sample that is less geographically varied. In contrast, our recruitment approach yielded a sample with greater geographical representation from across Spain. Second, being a community sample, diabetes related data, including glycated hemoglobin values were reported by parents. However, based on previous work with adults (Fisher et al., 2015), it is likely that most parents are also able to recall their children’s hemoglobin values reliably. Finally, relatively few fathers participated and the mean sample educational level was high, further limiting generalizability. This Spanish version of the PDDS has been designed for use in Spain and has been validated in the cultural and healthcare context of Spain. Future studies are needed to analyze its applicability in other Spanish-speaking countries. In conclusion, the PDDS-SP is a brief tool that effectively identifies parents’ concerns and fears which would make it easier to discuss them in clinical encounters (Fisher et al., 2019). The findings from this study suggest that the instrument demonstrates good validity and reliability within the sample assessed. Thus, PDDS-SP may be a useful tool for both research and Spanish health professionals as a starting point for conversations with parents about their concerns related to their child’s diabetes. Conflict of Interest The authors of this article declare no conflict of interest. ACKNOWLEDGMENT We thank Javier Hurtado and Iñaki Lorente for their help in recruiting participants for the study. Cite this article as: Beléndez, M., & Fisher, L. (2025). Validation of the Spanish Version of the Parent Diabetes Distress Scale. Clinical and Health, 36(1), 19-24. https://doi.org/10.5093/clh2025a3 References |
Cite this article as: Beléndez, M. & Fisher, L. (2025). Validation of the Spanish Version of the Parent Diabetes Distress Scale. Clinical and Health, 36(1), 19 - 24. https://doi.org/10.5093/clh2025a3
Correspondence: marina.belendez@ua.es (M. Beléndez).Copyright © 2025. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS







